Top 3 Chronic Mental Health Conditions Affecting Women In The USA
Here are three of the most prevalent chronic mental‐health conditions affecting women in the U.S., listed from most to less prevalent, along with why they disproportionately affect women and key notes for each.
1. Anxiety Disorders




Prevalence and gender difference
-
In the U.S., about 19.1% of adults had any anxiety disorder in the past year; prevalence was higher for females (~23.4%) vs males (~14.3%). (National Institute of Mental Health)
-
Women are more than twice as likely as men to develop an anxiety disorder over the lifetime. (U.S. Food and Drug Administration)
-
Among adolescents (ages 13-18) the lifetime prevalence of any anxiety disorder was ~31.9%, higher for females (~38.0%). (National Institute of Mental Health)
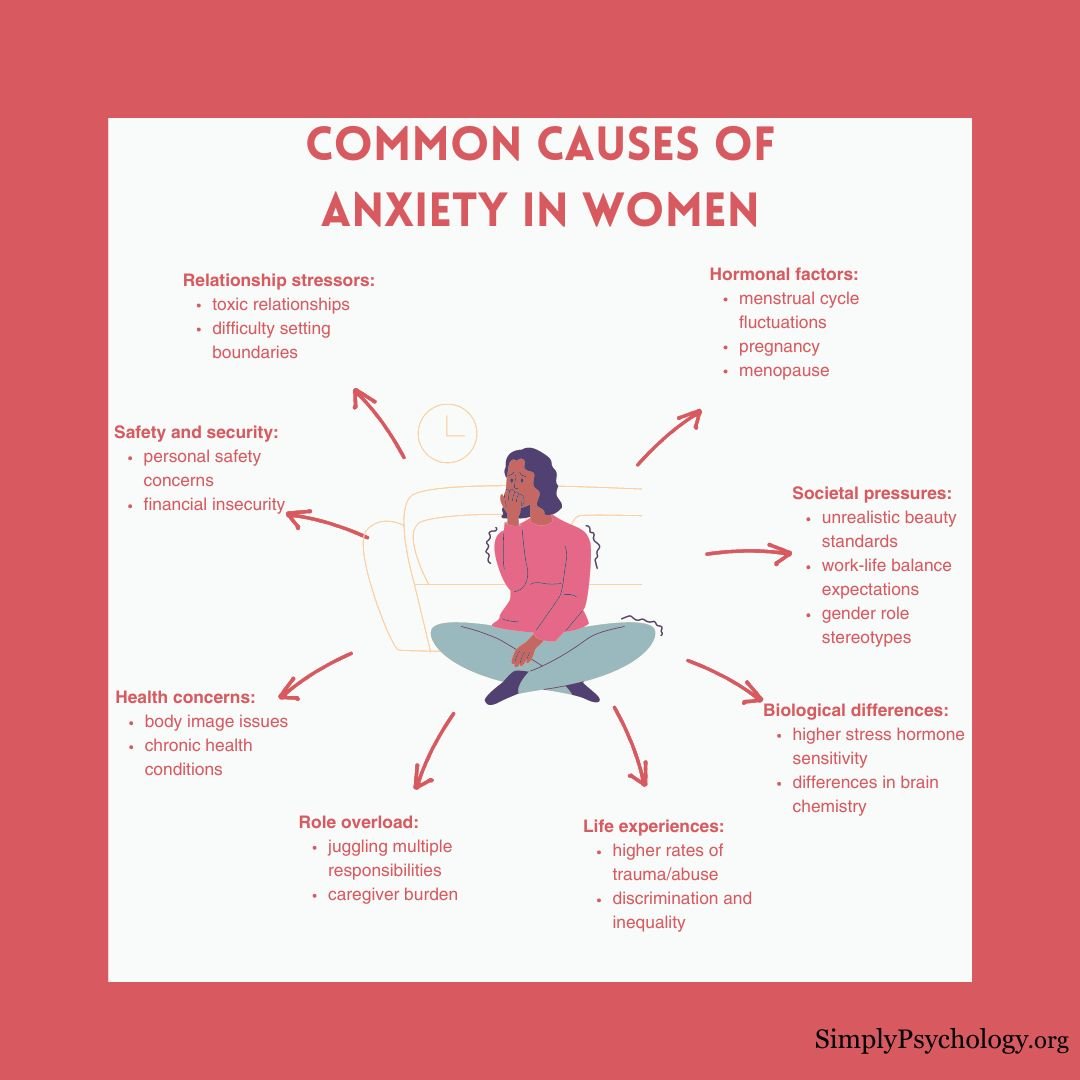
Why it matters for women
-
Anxiety disorders are the most common mental disorders overall, and because they are highly prevalent in women, they represent a major chronic burden. (Office on Women's Health)
-
Factors such as hormonal fluctuations (menstrual cycle, pregnancy/postpartum, menopause), social/role stress (family, caregiving, work) and exposure to trauma contribute disproportionately for women. (Office on Women's Health)
-
Chronic anxiety can lead to impaired daily functioning, comorbid depression, and increased physical-health risks (e.g., cardiovascular) when unmanaged.
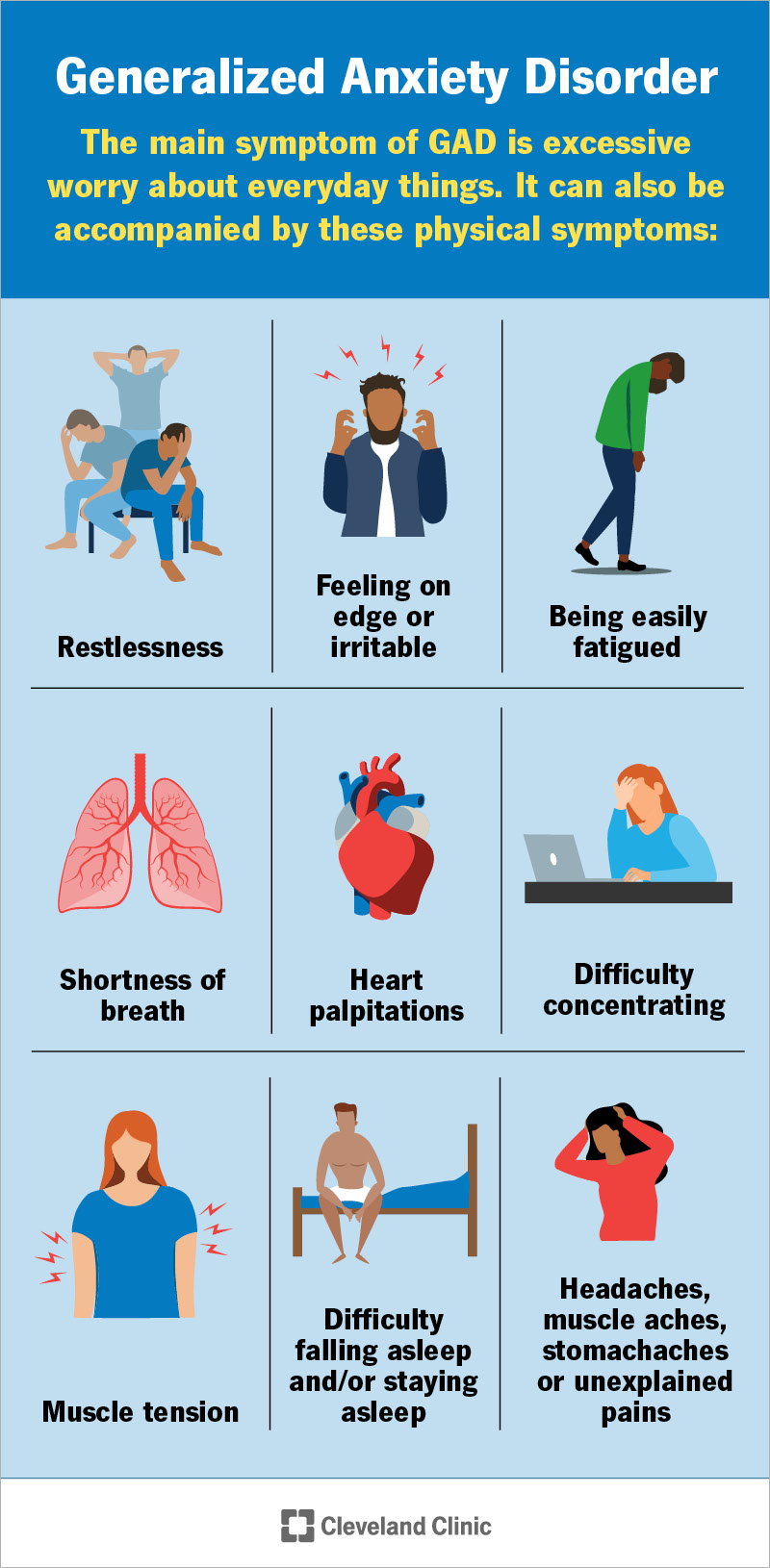
Key features
-
Includes disorders such as generalized anxiety disorder (GAD), panic disorder, specific phobias, social anxiety disorder, etc. (National Institute of Mental Health)
-
Treatment includes psychotherapy (e.g., CBT), sometimes medications, lifestyle/behavioral interventions. Early detection improves outcomes.
-
Because of high prevalence, screening in women (especially during transitions like pregnancy or menopause) is important.
2. Major Depressive Disorder (and Depressive Disorders)


Prevalence and gender difference
-
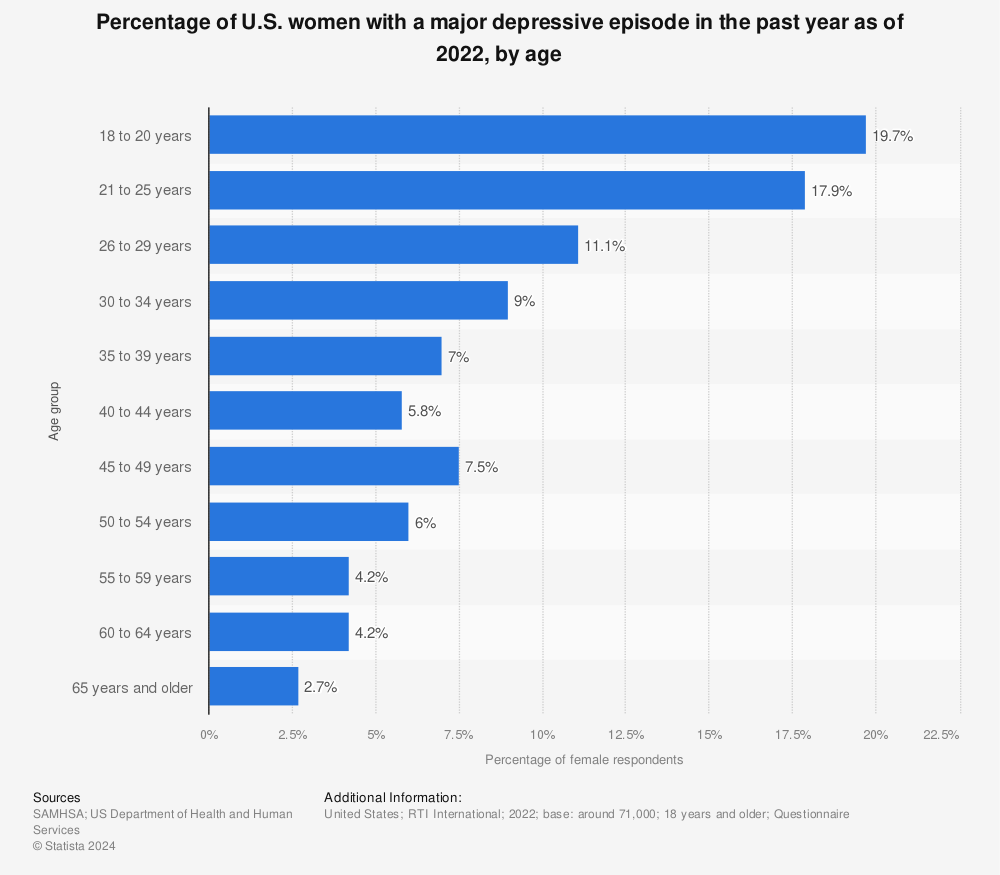
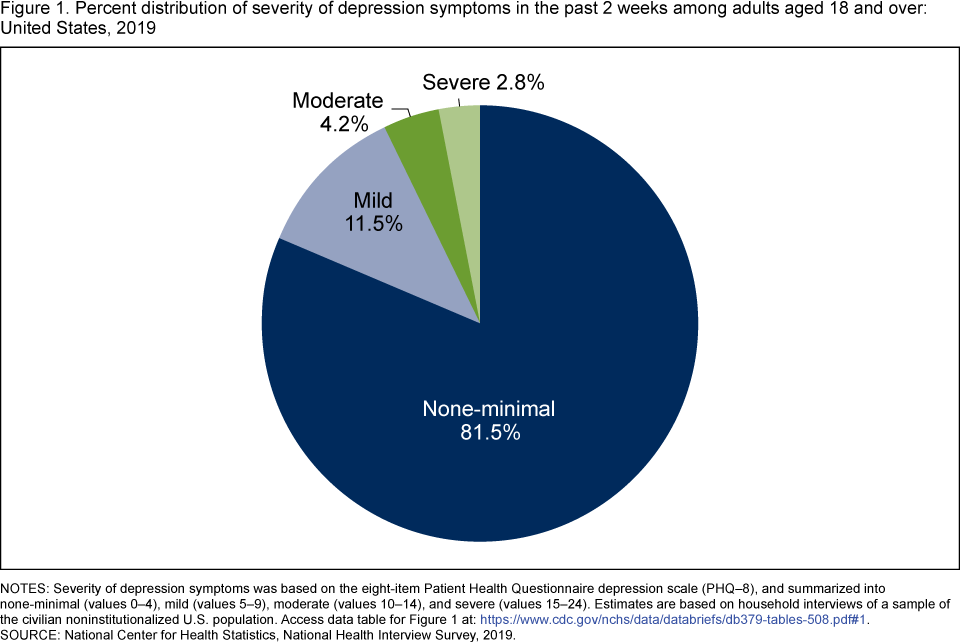
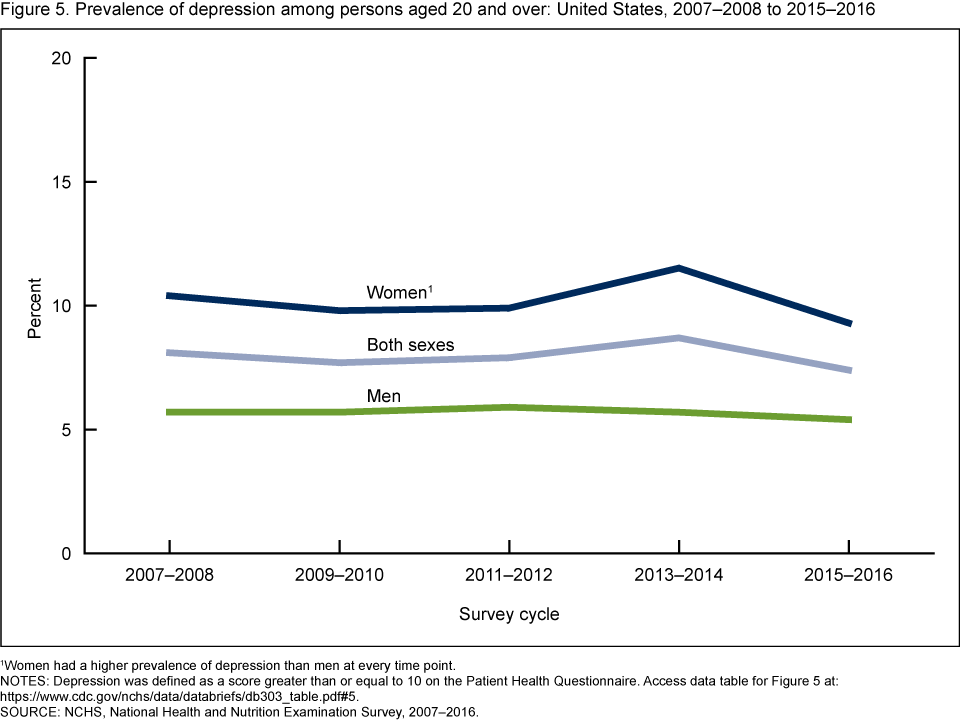
Current data show that roughly 13.1% of U.S. adolescents and adults aged 12+ had depression in a given 2-week period (Aug 2021–Aug 2023). Females had higher prevalence than males. (CDC)
-
More broadly, women experience depressive disorders at higher rates than men: for example, women are more likely than men to have a major depressive episode. (American Psychiatric Association)
Why it matters for women
-
Depression is a chronic condition in many cases—may recur or persist, and lead to significant impairment, thus qualifying as a major chronic mental-health burden.
-
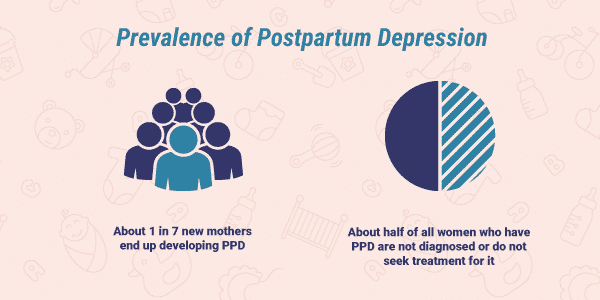
Women face additional risk contexts: postpartum depression, perimenopausal depression, societal/role stress, trauma/abuse exposure. (National Institute of Mental Health)
-
Depression in women is often under-diagnosed or undertreated; yet untreated depression contributes significantly to disability, reduced quality of life, and physical health comorbidity (e.g., heart disease).
Key features
-
Major Depressive Disorder (MDD) presents with persistent low mood, loss of interest or pleasure, and other symptoms for at least 2 weeks, with impact on daily functioning.
-
Chronic or recurrent depression often requires ongoing management: psychotherapy, medication, lifestyle approaches, support.
-
Because many women live with cycles of life changes (pregnancy, menopause), risk and management may need a more tailored/proactive approach.
3. Eating Disorders
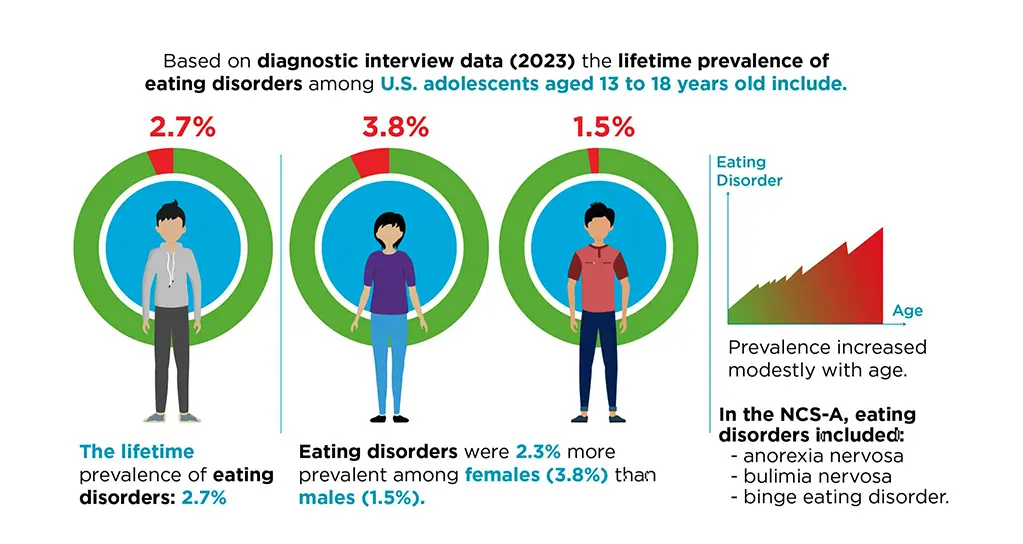

Prevalence and gender difference
-
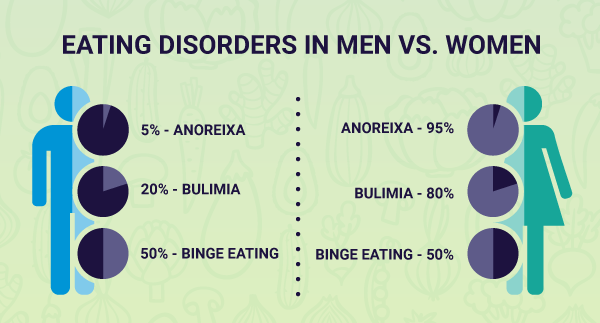
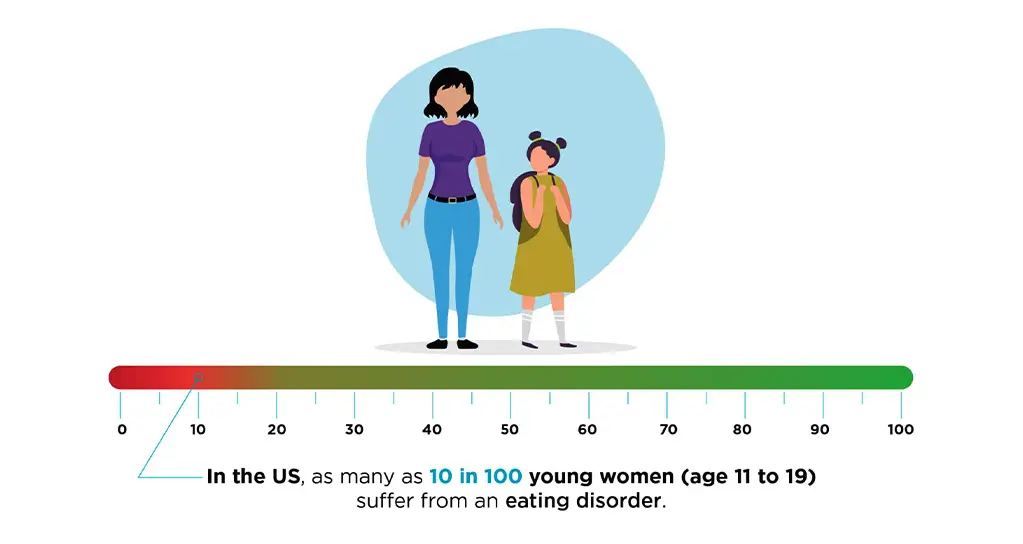
The lifetime prevalence of eating disorders among females in the U.S. is estimated at ~8.60% (versus ~4.07% in males) according to data from the National Eating Disorders Association. (National Eating Disorders Association)
-
For example: approximately 3.5% of women will have binge eating disorder in their lifetime. (Eating Recovery Center)
Why it matters for women
-
Eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder, OSFED/other specified feeding or eating disorders) disproportionately affect women and often become long-term/chronic without appropriate treatment.
-
They often begin in adolescence or young adulthood and can persist into later life, causing physical complications (nutritional deficiencies, cardiac issues), psychological comorbidity (depression, anxiety) and high mortality risk (especially anorexia). (ANAD)
-
Because they often are hidden, under-recognized, and stigmatized, they may become chronic before being addressed.
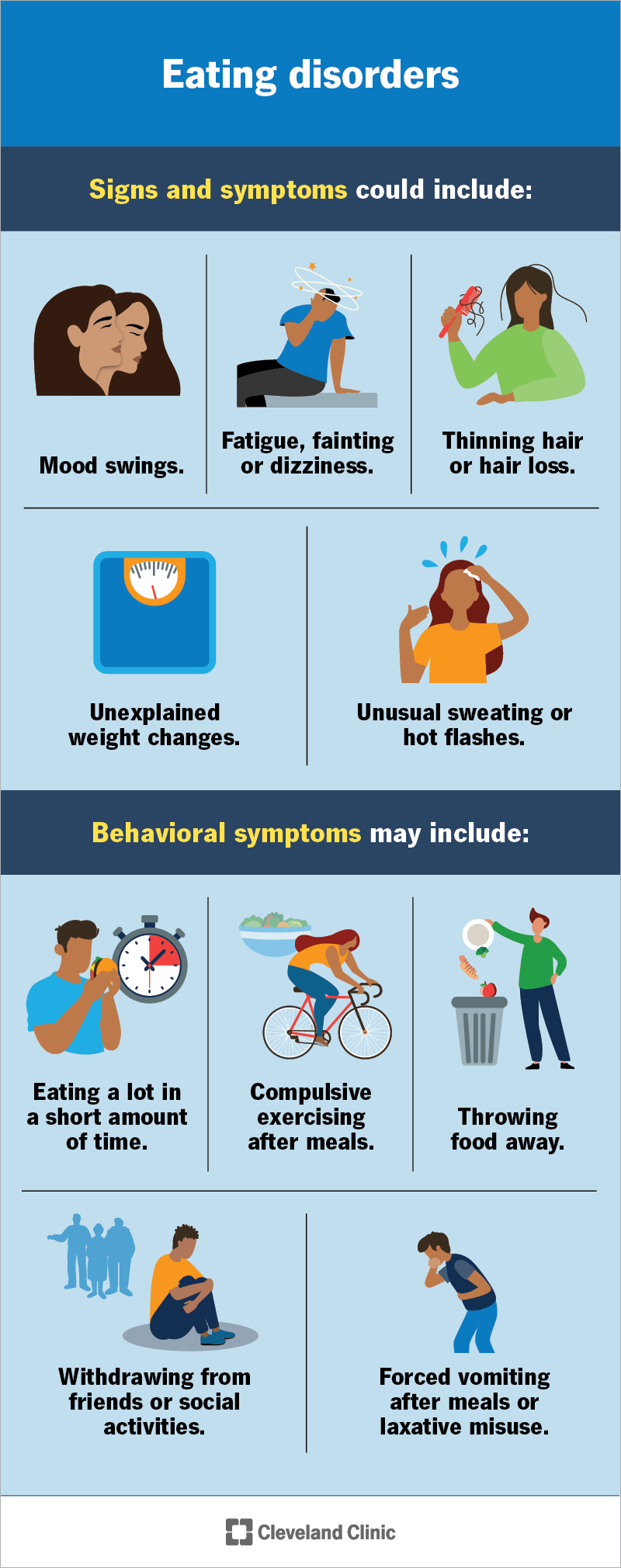
Key features
-
Types include: anorexia nervosa (restriction of energy intake), bulimia nervosa (bingeing + compensatory behaviors), binge eating disorder (recurrent binge eating without compensatory behaviors), and other specified feeding or eating disorders (OSFED). (American Psychiatric Association)
-
Management involves multi-disciplinary care: medical monitoring, nutritional rehabilitation, psychotherapy (CBT, DBT), sometimes medications.
-
Because of the high female burden and long-term risk, eating disorders are a major chronic mental-health concern for women.
Summary Table
| Rank | Condition | Approximate female prevalence / gender notes | Why it’s a top chronic mental-health burden for women |
|---|---|---|---|
| 1 | Anxiety Disorders | ~23.4% of U.S. adult females in past year had any anxiety disorder. (National Institute of Mental Health) | Most common mental-health condition; high prevalence + chronic potential |
| 2 | Depressive Disorders (Major Depression) | ~13% of U.S. adolescents/adults (12+) had depression in a 2-week span; higher in females. (CDC) | High burden, chronic or recurrent nature, strong female risk factors |
| 3 | Eating Disorders | ~8.6% lifetime prevalence among women vs ~4% among men. (National Eating Disorders Association) | Disproportionate female impact, onset in youth, chronic course if untreated |
Final Notes
-
These three conditions overlap frequently: e.g., anxiety + depression are highly comorbid; eating disorders often coexist with anxiety or depression.
-
“Chronic” means ongoing, long-term, or recurring — all three conditions meet that in many women, not just one-time episodes.





No comments:
Post a Comment